Happy Birthday Kehlani
October 29, 2020
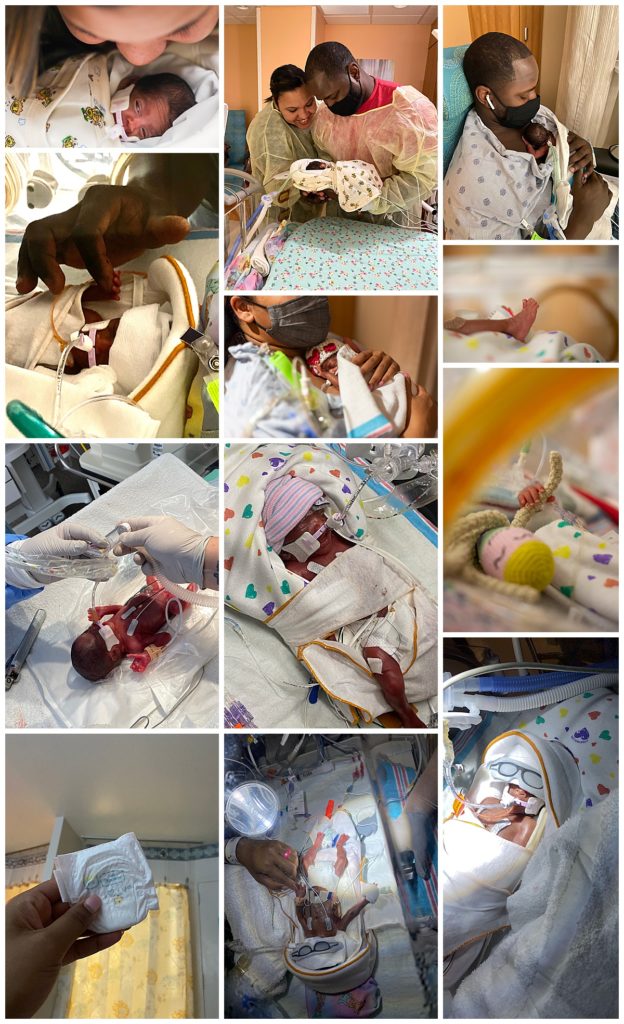
After making it to 21 weeks they ended up sending me home on strict bed rest to wait it out even longer and told me to return if I had any changes or felt like something didn’t feel right to come back in. The day I turned 22 weeks I kept feeling Kehlani kick really low to the point where it felt like she was kicking me in my vagina (sorry to be so blunt! Didn’t know how else to describe it). It was around 11pm and I told my husband Lewis that something just didn’t feel right and we need to go back into the hospital just to make sure things are ok. So we got ready and took the hour drive back to the high risk hospital for evaluation. They did an ultrasound and told me that Kehlani had turned feet down (breech) from the last time I was there and her feet was kicking right where my sack was bulging through my cervix and because I was dilated I could feel her kicks much lower. Then they came back with the entire high risk team and once again presented us with some options. They said that since we now made it to 22 weeks we now have the choice as to whether or not we would like to resuscitate her if she delivered at 22 weeks. They gave us all the scary statistics about what kind of long term physical disabilities she could have should we decide to resuscitate her that early and how under developed all her organs will be. To be honest when I look back all of their “advice” feels like they want you to NOT resuscitate your baby and honestly that is something that should change. Although I understand needing to make us aware of the negative possibilities, I feel they should equally encourage parents of the positive stories and outcomes as well, not just the bad. Both my husband and I instantly told them that no matter what we wanted them to perform life saving measures on her at all costs if she is born any time from that day forward. The next decision they faced us with was treatment for her brain and lung development. They wanted to admit me that night into the hospital to begin steroid injections to help her lung development and magnesium treatment through an IV that helps to protect her brain if delivered early. They told me that if I agreed to receive the treatment I would have to be admitted into the hospital indefinitely until she was born. We asked them for some private time to talk it over, and the most difficult decision for us was the fact that we didn’t know how long I would be in the hospital and we had a son at home who is on the spectrum with severe separation anxiety when he’s away from me and he’s not allowed to visit me in the hospital due to the covid precautions. So I just couldn’t agree to begin treatment that night without going home first and preparing the kids especially our son that I would be leaving again for an unknown time. We also had to figure out child care for our kiddos especially since Lewis’ mom who had flown in to help us was leaving to go back home in just a few days. We ended up telling the doctors that we needed a week to get things together and that we will try to come back at 23 weeks for treatment. Three days before I turned 23 weeks I had an OB appointment at the office where one of the high risk specialist said to me “it is my professional opinion that you go in at 23 weeks and get this treatment immediately”. I said ok, I promise I will go in and begin it at 23 weeks. She also told us that she would speak to the hospital manager about my son having anxiety and see what they can do to help. Three days later we packed up everything for a long term hospital stay and headed on in. This was a Sunday and that day I was officially 23 weeks. They began steroids and magnesium within an hour of me being admitted. Due to the magnesium being a muscle relaxer I wasn’t allowed to walk once it began and they told me the treatment takes 48hrs to complete. So for two days I had to pee in a bed pan which I HATED! Mostly because I felt well enough to walk to the bathroom! But they just don’t want to risk you losing your balance and fall. That morning the hospital manager came to my bedside to talk to me about my son and granted us an exception to policy to where my son could come and visit me in the hospital whenever he wanted and listed his sister has his support person so that she could come too. This was a huge emotional relief for our entire family. I can’t say enough good things about the staff, doctors, and nurses that do everything they can to make a bad situation bearable. The doctor who originally told us we were losing her at 20 weeks came in to see me that afternoon and said that he was concerned with Kehlani being breech. The concern was if my water broke the cord can become exposed immediately and can cut off her oxygen supply and kill her before they can get her out. Then he said it’s typically better to go in and take the baby out BEFORE that situation happens. Of course I wasn’t ok with this option at all because I wanted to keep her in as long as possible. So he said they will take an ultrasound of the baby to try and gage how much she weighs and then talk to neonatology about what to prepare for with delivery. Last minute in the middle of the night before the doctor went home he told my nurse not to let me eat or drink anything after midnight, which they said is typically only done when they are planning for a procedure the next day. So all night I felt anxious that they were going to try to convince us to have her the next day. So I prayed begging god that they will not try to force labor in the morning. The next morning a different doctor was on shift for the day and he came in and said exactly what I prayed for, he said “I don’t want to risk having the baby earlier than needed, I feel like you have all the specialist right here if your water breaks and I think we can get to you quickly if that happens. If I can keep the baby inside of you as long as I can that’s what I want to do”. I felt so relieved! Not only that but by that afternoon I had completed the 48hr treatment, I was able to eat and I could get up and go to the bathroom! However, this high of relief didn’t last very long. The next morning (in the middle of the night) at 1:30am at 23 weeks and 3 days on October 14th I was sound asleep when I woke up to water just gushing out of me. For a second I thought I was peeing on myself, then I realized what was happening, My water had broken. I called my nurse and told her my water broke. Then I grabbed my phone and texted my husband to get to the hospital because I think my water broke. Then I called him and told him my water broke. I stayed completely still on my side exactly how I was when I woke up because I was scared to move and scared for the cord to become exposed. I began shaking uncontrollably and crying. One of the OBGYN’S came in and she checked me while on the phone with the high risk specialist, I heard her say to him “no I don’t feel or see a cord, but the baby’s feet are out, do you want me to hold the feet in until we get in the operating room or do you think its ok to just wheel her in”. Then she hung up and said to me while wheeling me out of my room “ma’am, your water has broken and your baby’s feet are out and kicking, we have to move to an emergency c-section right away”. All I could think about was if neonatology was called and all I got out was “did someone call neonatology?” and I heard someone say “yes they are on their way to the operating room now”. Everything else moved so fast, before I could even think about what was next I was in the operating room on the table, a nurse grabbed my phone from me and asked if she had permission to take pictures and videos on of the baby when she’s born, which I was so grateful for because I didn’t even know if Kehlani would be alive when I woke up and if I would ever see her alive. So I gave the nurse my password and said yes please thank you! The anesthesiologist tried to do her best to calm me, she was rubbing my shoulders trying to help me relax but I couldn’t stop shaking uncontrollably. The anesthesiologist did her best to tell me everything that was happening to me before it happened. They shove the catheter in you before you’re put to sleep, shave the surgical area, sanitize it all while the doctor is scrubbing in. So you just feel a bunch of people doing things to you and you’re just laying there unable to do anything about it. I heard a guy yelling out all the tools that were laid out. Then in came the neonatal team and right after my doctor walked in. She came to the right side of me and did a roll call to make sure everyone was there really quickly and then looked at the anesthesiologist and said “were ready” next thing I know I woke up. I couldn’t talk but I could hear and I could hear Lewis’ voice and then I could hear the neonatologist say “Hi, I’m the neonatologist”. I wanted so bad to say “how is she?!” but I couldn’t speak, however almost on cue I hear Lewis say “How is she?” which to this day makes me feel like were so connected haha! Then I hear the doctor say “she’s actually doing good and she’s stable and were getting her set up in her pod now and you can go see her real soon”. It was the best thing I could have heard after waking up. I will say having general anesthesia vs a spinal or epidural is the WORST. You wake up in instant pain. I was crying because I was in so much pain when I woke up and felt like the “hard core drugs” they were giving me wasn’t working at all. They also have to push on your stomach like every like 15 mins or so to make sure you aren’t clotting and my god it was the worst pain ever! After they got me settled back into my room Lewis went to go see Kehlani for the first time and check on her. When he returned I asked him if I could see a picture of her and after seeing her I just cried because she was ALIVE. God did it, we did it, all of your prayers did it, God saved her. He granted us grace and found us worthy and save our 1lb 7oz baby girl!
Leave a Reply Cancel reply
MVP
HOME
ABOUT
WEDDINGS
VIDEOGRAPHY
INVESTMENT
ENGAGEMENTS
GALLERIES
PORTRAITS
BLOG
CONTACT
Freezing time so that YOUR memories last a lifetime!
© MCNEAL VIDEO AND PORTRAITS 2023